Modern Antimalarial Drug Technology: How Plant-based Nanotechnology Has Emerged as a Promising Mechanism for Preventative and Curative Treatment of Malaria
- Amanda Benneh
- Jan 14, 2025
- 6 min read
Written by: Amanda Benneh
Edited by: Jessica Kim and Gerard Murillo
Illustrated by: Toni Chavez

Introduction
In the face of the devastating global malaria crisis, the search for effective treatments to prevent and cure the disease in patients is a priority for the medical field. Researchers are making significant progress by merging biology and nanotechnology to target and reduce malaria transmission effectively [1]. Malaria is a life-threatening disease caused by the Plasmodium parasite, which is transmitted to humans through the bite of an infected Anopheles mosquito [2]. According to the World Health Organization 2023 World Malaria Report, there were over 249 million cases of malaria across 85 countries in 2022, with 58 cases per 1000 population at risk [2]. Of these malaria cases, 95% occurred in the WHO African Region, particularly in countries like Nigeria, the Democratic Republic of the Congo, Uganda, and Mozambique [2]. As such, malaria is most prevalent in Sub-Saharan Africa and South Asia, where tropical conditions such as high rainfall and humidity form an ideal environment for the growth and development of Anopheles mosquitoes that spread the Plasmodium parasite [3]. Today, research shows a promising future in plant-based nanotechnology that targets infected female Anopheles mosquitoes, enhancing drug delivery and controlling malaria transmission [4].
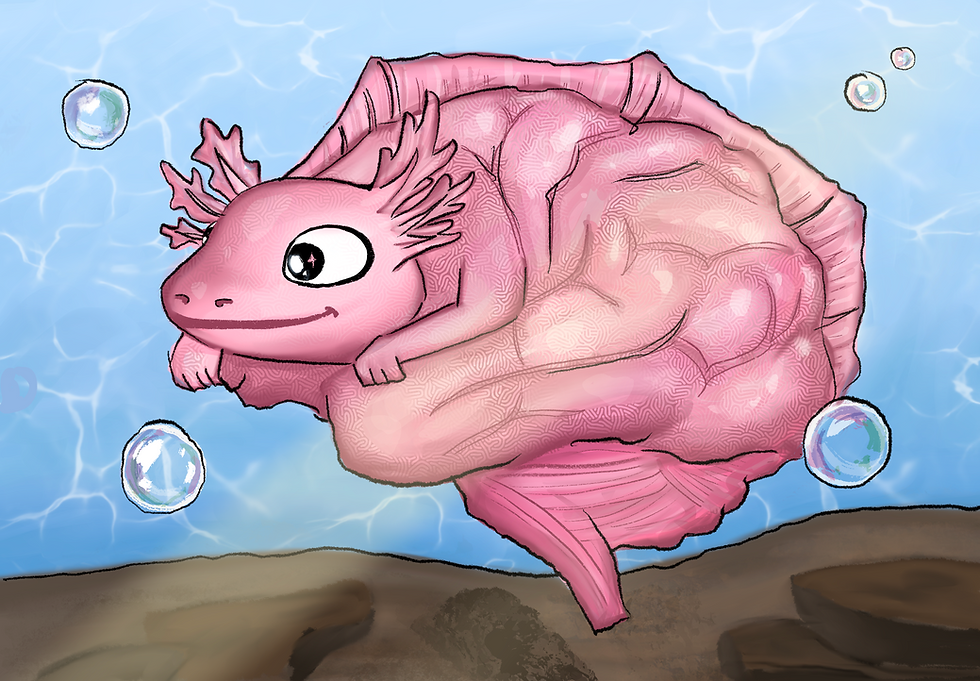
The Plasmodium parasite species have a complex life cycle in humans following a bite from an infected mosquito [5]. Sporozoites, the first stage of the parasite’s life cycle, infect liver cells and reproduce over 7-10 days [5]. The parasites then burst from the liver cells and enter the bloodstream, where red blood cells are infected, and parasite cells continue to rapidly divide and rupture [5]. This asexual replication causes the clinical symptoms of malaria, such as fever, chills, and nausea, due to the accumulation of waste products and the subsequent immune response [5]. The lack of access to proper diagnostic tools and resources for vulnerable populations can delay malaria treatment and lead to more severe complications from its clinical symptoms [6].
The best first-line treatment for malaria caused by Plasmodium falciparum is an artemisinin-based combination therapy [ACT] [7]. ACT consists of two drugs, artemisinin and a partner drug, that collaboratively target multiple pathways of parasite growth in red blood cells [7]. However, current treatments, including ACT, are becoming less effective due to the parasite’s growing resistance to antimalarial drugs [7]. While original preventive measures—vaccines and drugs—are becoming less effective, plant-based nanotechnology offers a promising approach to enhance drug delivery and reduce malaria transmission [8].
Background: Nanotechnology
Nanotechnology involves manipulating materials on a molecular level, typically between 1 to 100 nanometers [3]. Nanoparticles [NPs], the fundamental elements of nanotechnology, are synthesized from various organic or “green” materials, including vitamins, proteins, lipids, carbohydrates, botanical extracts, biodegradable polymers, and microorganisms [7]. Metallic nanoparticles, including silver, gold, and iron oxide, have unique properties that make them useful in various pharmaceutical and medical applications [9]. Previously, metallic nanoparticles have been synthesized through chemical processes such as chemical vapor deposition, co-precipitation, thermal evaporation, vaporization, and radiolysis [9]. These processes were energy-intensive and produced toxic byproducts [9]. To address this, scientists turned to “green” synthesization that only involves living organisms such as bacteria, fungi, plants and viruses, and other biomolecules, including vitamins, enzymes, proteins, peptides, monosaccharides, polysaccharides, and polymers [9]. The development of NPs through these methods allows scientists to access materials that are cost-effective and sustainable while reducing the potential for toxicity and energy waste [9]. Plant-based metallic NPs differ in their properties and uses [7]. For instance, silver NPs, made from plant extracts like Artemisia, which is also used in antimalarial drugs, have antibacterial effects that can target malaria-causing parasites [9]. Research shows that silver NPs, derived from plant extract, can kill parasites in infected human red blood cells and mouse models [9]. Iron oxide NPs are biocompatible, non-toxic, and can work in conjunction with other antimalarial drugs [9]. Green-synthesized nanoparticles are an eco-friendly alternative to chemically synthesized nanoparticles that exhibit high toxicity on eukaryotic cells, allowing for more flexibility in their preventive applications [7].
Nanotechnology in Drug Delivery Systems
Previous research in malaria treatment focused on the promising applications of nanotechnology in drug delivery systems [10]. Nanoparticles carry drugs directly to the parasite vacuole, a cell organelle responsible for storing waste products, and maintain drug levels in the bloodstream for extended periods while reducing toxicity [9]. These nanocarriers, synthesized by a diverse range of biomolecules, are used with standard antimalarial drugs, including artemisinin and its derivatives [9]. Lipid-based NPs and liposomes are primary candidates in nano-drug delivery systems due to their bioavailability and ability to increase antimalarial drug and vaccine efficacy [9]. Liposomes are vesicles formed by the entrapment of fluid by phospholipid molecules, which have hydrophobic and hydrophilic components that form bilayers, allowing it to act as a vehicle for drug delivery [10]. Scientists can modify the liposome bilayer to incorporate antimalarial drug molecules within the liposomes to deliver them into infected human cells [10]. Studies show this method improves targeted drug delivery, protecting the drug from degradation and reducing the frequency and dosage of administration [9]. However, lipid-based nanoparticles can be limited by their synthetic chemicals, triggering unwanted immune responses in humans [10]. This led the researchers to explore the use of plant-based metallic NPs, which are safer and more sustainable [7].
Plant-Based Nanoparticles Applications in Malaria Prevention and Treatment
Plant-based metallic nanoparticles can be used to target and control mosquitoes infected with Plasmodium to reduce transmission of the disease before human infection [9]. Due to their synthesis using biodegradable, non-toxic, and cost-effective materials, green nanoparticles that kill mosquitoes can be sustainably produced using plant extracts [9]. Metallic NPs can hinder larvae and pupae development, altering their life cycles and lowering mosquito populations when placed into mosquito breeding areas in warm climates [9]. Silver NPs show the highest success in targeting mosquitoes at the larval stage when tested against species of malaria-carrying mosquitoes, which is important for mosquito control in highly endemic areas like Sub-Saharan Africa [9]. In addition to vector control, green metallic nanoparticles, including silver, iron, and gold, have potential activity against Plasmodium species due to their advantageous properties [9]. Research shows that silver NPs derived from various plant extracts inhibit the molecular process underlying the growth and reproduction of Plasmodium parasites [9]. Silver nanoparticles can target different stages of the parasite’s life cycle, especially during the blood stage of infection [5]. Similarly to silver NPs, gold NPs are biocompatible and have high binding activity to surface proteins of P. falciparum, making them good candidates for drug delivery systems [9]. Lastly, iron oxide NPs can aid the activation of artemisinin-based combination therapy, which is metabolized in the presence of the Fe2+ ions [7]. Iron Oxide NPs, and other metallic NPs, can combat parasite resistance to first-line antimalarial drugs and avoid the potential of non-activation in parasite cells [9].
Conclusion
The alliance between nanotechnology and microbiology offers exciting perspectives in antimalarial treatment and drug research with its ability to control malaria vectors and enhance antimalarial treatment in recent studies [10]. Plant-based nanoparticles in malaria research will contribute to the control, prevention, and treatment of the disease, and combat antimalarial drug resistance in Plasmodium parasite species [9]. This “green” approach to nanotechnology could be the answer to combating malaria transmission in highly endemic countries, replace existing antimalarial therapies, and potentially be applied to other diseases in the future.
References
[1] Rahman, K., Khan, S. U., Fahad, S., Chang, M. X., Abbas, A., Khan, W. U., Rahman, L., Haq, Z. U., Nabi, G., & Khan, D. (2019). Nano-biotechnology: a new approach to treat and prevent malaria. International journal of nanomedicine, 14, 1401–1410. https://doi.org/10.2147/IJN.S190692
[2] Venkatesan, P. (2024). The 2023 WHO World malaria report. The Lancet Microbe, 5[3], e214. https://doi.org/10.1016/S2666-5247[24]00016-8
[3] National Center for Emerging and Zoonotic Infectious Diseases (NCEZID). (n.d.). Where malaria occurs. Retrieved from https://www.cdc.gov/malaria/data-research/index.html
[4] Lokole, P. B., Byamungu, G. G., Mutwale, P. K., Ngombe, N. K., Mudogo, C. N., Krause, R. W. M., & Nkanga, C. I. (2024). Plant-based nanoparticles targeting malaria management. Frontiers in pharmacology, 15, 1440116. https://doi.org/10.3389/fphar.2024.1440116
[5] Enugopal, K., Hentzschel, F., Valkiūnas, G., et al. (2020). Plasmodium asexual growth and sexual development in the haematopoietic niche of the host. Nature Reviews Microbiology, 18 (2), 177-189. https://doi.org/10.1038/s41579-019-0306-2
[6] Jia, L., Chen, X., Feng, Z., Tang, S., & Feng, D. (2024). Factors affecting delays in seeking treatment among malaria patients during the pre-certification phase in China. Malaria journal, 23 (1), 73. https://doi.org/10.1186/s12936-024-04892-4
[7] Nosten, F., & White, N. J. (2007). Artemisinin-based combination treatment of falciparum malaria. In J. G. Breman, M. S. Alilio, & N. J. White (Eds.), Defining and Defeating the Intolerable Burden of Malaria III: Progress and Perspectives: Supplement to Volume 77 (6) of American Journal of Tropical Medicine and Hygiene. Northbrook, IL: American Society of Tropical Medicine and Hygiene. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1713/
[8] Murthy S. K. (2007). Nanoparticles in modern medicine: state of the art and future challenges. International journal of nanomedicine, 2(2), 129–141.
[9] Barati, A., Huseynzade, A., Imamova, N., Shikhaliyeva, I., Keles, S., Alakbarli, J., Akgul, B., Bagirova, M., & Allahverdiyev, A. M. (2024). Nanotechnology and malaria: Evaluation of efficacy and toxicity of green nanoparticles and future perspectives. Journal of Vector Borne Diseases, 61(3), 340-356. https://doi.org/10.4103/JVBD.JVBD_175_23
[10] Keleş, S., Alakbarli, J., Akgül, B., Baghirova, M., Imamova, N., Barati, A., Shikhaliyeva, I., & Allahverdiyev, A. (2024). Nanotechnology based drug delivery systems for malaria. International Journal of Pharmaceutics, 666, 124746. https://doi.org/10.1016/j.ijpharm.2024.124746


Comments